- Surgery
- January 29, 2026
- 5 MINS READ
Dr. P. C. Vijayakumar
MBBS, DA, DNB (Anaesthesiology), MNAMS
Chief Anaesthesiologist & Director- Academics
Dr Latha Poopandian
MBBS, DA, EDAIC, CCEBDM, Fellowship in Critical care Nutrition
Anesthesiologist
Dr. A. Bhuvaneswari Anandhakumar
D. A., EDAIC
Anesthesiologist
A 60 year old gentleman with a long history of heavy smoking and alcohol use came to us with severe breathing difficulty. His scan showed right lower lobe collapse consolidation and he was in Type 1 respiratory failure, meaning his lungs were not able to deliver enough oxygen to the body. Cases like these are exactly why we take breathing problems in smokers seriously, because the situation can worsen very quickly and not always for the obvious reasons.
When someone comes in like this, the first thought is usually infection or mucus plugging, but it is not always that simple. There are many persistent breathlessness causes, and if symptoms keep getting worse even with oxygen and treatment, it is a sign that something deeper may be happening inside the airway.
Why We Chose Bronchoscopy on NIV
Instead of immediately putting him on a breathing tube, we decided to do a bronchoscopy while he continued on NIV support. This approach, known as bronchoscopy on NIV, is not for every patient, but it can be extremely helpful when the lungs are fragile and you want to avoid the extra risks that come with intubation.
We performed it as an awake bronchoscopy, so the patient could maintain natural breathing and we could assess the airway in real time. In the right setting, it is safer, controlled, and also gives answers faster compared to waiting and watching while the patient struggles.
Here is why this technique made sense in his case:
- it preserves natural breathing
- it avoids the risks of intubation
- it helps us directly see what is blocking the airway
- it allows immediate suctioning or clearing if needed
What We Found Inside the Airway
During bronchoscopy, we found large amounts of thick pus completely blocking his airways. It was not a small plug, it was enough to restrict airflow significantly. Once we cleared it out, the improvement was immediate, and this itself became a major part of his difficulty breathing treatment because the obstruction was acting like a physical barrier inside the airway.
But even after clearing the pus, something still looked unusual in the way his windpipe behaved during breathing. That was the moment we realised we might be dealing with something beyond infection, and that is where the real tracheomalacia diagnosis started becoming clear.
A Rare Diagnosis: Adult Tracheomalacia
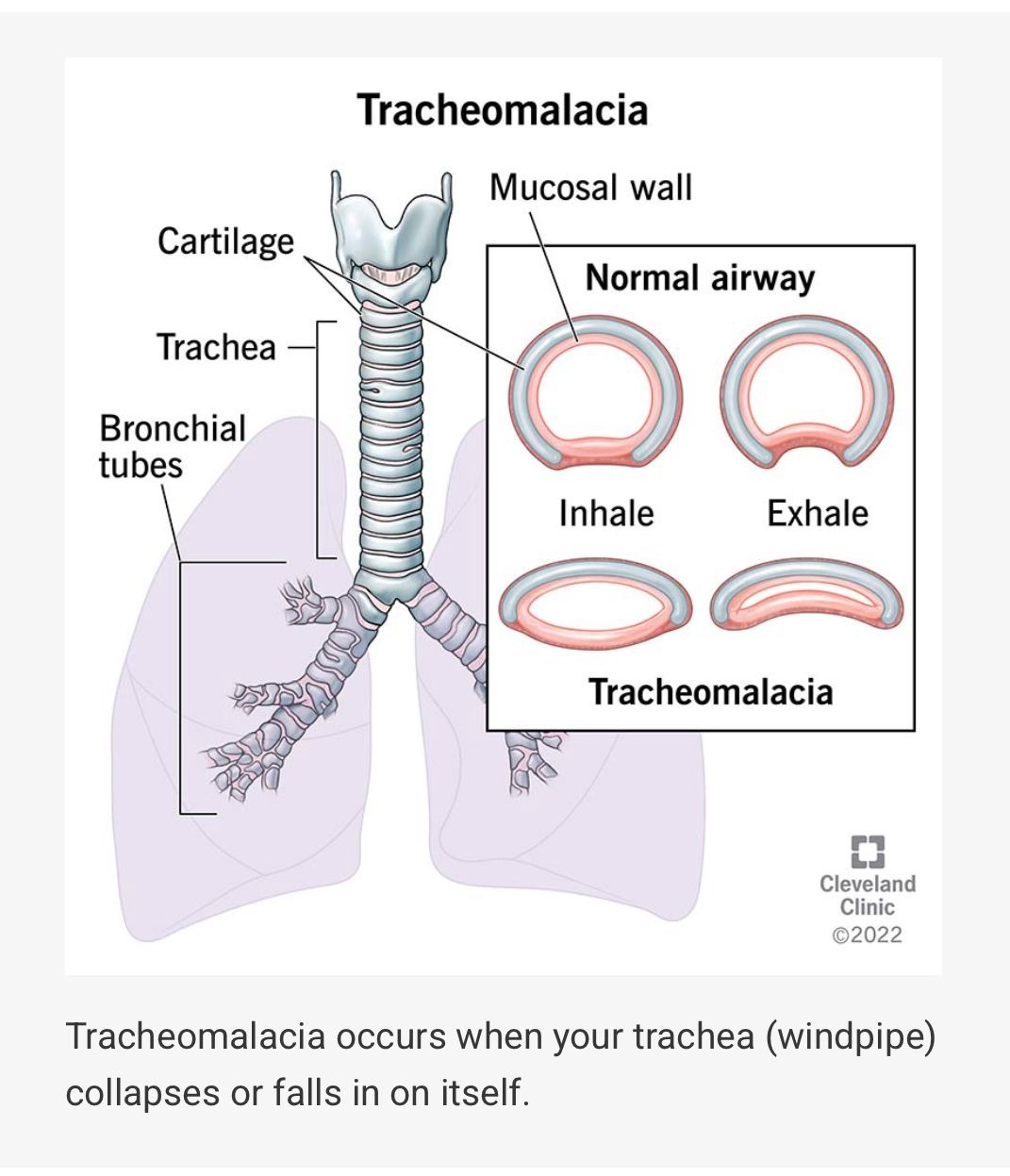
The most unexpected finding was adult tracheomalacia, a rare condition where the trachea becomes soft and collapses during breathing instead of staying open. It is not commonly diagnosed in adults, and many times it gets mistaken for other lung conditions, especially when the patient already has smoking history or infection.
In his case, the trachea was collapsing during expiration and even during inspiration, giving the classic crescent shaped appearance that doctors look for in tracheomalacia in adults. This collapse explained his high work of breathing, dependence on NIV, and the persistent airflow obstruction that was not improving as expected.
A few things this finding explained immediately:
- High work of breathing even on support
- Difficulty coming off NIV
- Ongoing obstruction like symptoms
- Breathlessness that seemed “too severe” for just consolidation
Why Did This Happen?
For this patient, the most likely reason was long term smoking. Years of irritation and inflammation can weaken the cartilage rings that keep the windpipe firm and open, and over time it can lead to adult tracheomalacia even if the person never knew anything was wrong earlier.
Not every smoker develops this, but smoking can quietly damage the airway in multiple ways. And when infection or mucus plugging happens on top of it, the symptoms become much more intense, which is why breathing problems in smokers should never be ignored or delayed.
Why This Case Matters
The reason this case is important is because tracheomalacia is uncommon and often missed. Many people assume breathlessness is “normal” after years of smoking, or they get treated repeatedly for infection without checking deeper. Understanding the real persistent breathlessness causes can completely change how a patient is managed and how safely the airway is handled.
This case also shows the value of using bronchoscopy on NIV, because it helped us identify a hidden airway issue without pushing the patient into invasive ventilation immediately. For the right patient, it can be a safer approach and gives direct answers when time matters.
Takeaway for Patients
If someone has ongoing breathlessness, frequent chest infections, or symptoms that keep coming back, it should not be ignored. Early evaluation can catch serious problems early, and in some cases, it can even detect rare conditions like tracheomalacia in adults before they become dangerous.
A few simple reminders:
- Do not ignore persistent breathlessness
- Get evaluated early instead of waiting
- Bronchoscopy can help diagnose airway blockages and structural issues
- Long term smoking can affect the airway, not just the lungs
In the end, clearing the thick pus helped immediately, but finding the underlying issue made the bigger difference. That is what made this more than just infection management, and why the final tracheomalacia diagnosis mattered for long term planning and care. At Sooriya Hospital, we believe timely airway evaluation can prevent delays and improve outcomes in complex breathing cases.


